[ad_1]
How well did payers provide “fair” access policies? Based on a recent ICER report titled “Assessment of Barriers to Fair Access”, the headline figures seem pretty good:
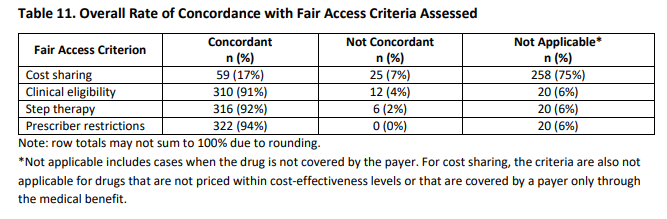
Overall rates of concordance with ICER’s criteria were 70% for cost sharing of fairly-priced drugs, 96% for clinical eligibility criteria, 98% for step therapy, and 100% for provider restrictions
At first glance, this seems like very fair access. However, digging a bit deeper, shows that patients do still face significant hurdles.
The table below shows that while 70% of drugs received fair access, this is based on the 84 drugs that were actually covered by insurance. Of the 342 drugs evaluated, however, most drugs (75%, 258 out of 342) were not covered at all. De facto, this means that cost sharing was 100%! If we include both covered and non-covered drugs in the analysis, then cost sharing would be considered fair based on ICER’s criteria only 17.4% (n=59 out of 352) of the time.
Payers were more likely to follow ICER rules with respect to clinical eligibility and limitations on step therapy, and provider restrictions. However, some of these fairness criteria represent a relatively low bar. For instance, ICER states that they have implemented “a maximum number of three steps allowed for a step therapy policy to remain concordant with fair access criteria”. Requiring patients to step through 2 let alone 3 therapies, however, is highly problematic for many diseases.
In short, do US commercial payers provide fair access? The answer to this question probably depends on the eye of the beholder.
[ad_2]
Source link