[ad_1]
Many people believe that the reason they feel out of sorts after a period of intense training is that they’re “overtraining.”
In reality, though, this is usually more the result of under-eating than overtraining.
Failing to fuel your body adequately when you’re highly active leaves you raddled.
Scientists call this low energy availability.
What is low energy availability, how do you calculate it, what happens when it goes unchecked, and how can you remedy it?
Get evidence-based answers to these questions and more in this article.
What Is Low Energy Availability?
Energy availability refers to the amount of energy the body has remaining to perform bodily functions after subtracting the energy you burn during exercise.
Thus, low energy availability describes a state in which your body doesn’t have enough energy to maintain optimal health and performance because you’ve burned too much energy exercising, consumed too few calories, or a mix of both.
Low energy availability in athletes is common, particularly among those who manipulate their weight for competition or for whom leanness or lightness is preferable (wrestlers, martial artists, bodybuilders, gymnasts, ballerinas, long-distance runners, jumpers, and so forth) because they typically limit their food intake and continue to train hard.
That said, it’s also prevalent among non-athletes. For example, people who begin exercising without adjusting their calorie intake, those looking to lose weight, and those with an eating disorder such as anorexia nervosa are all at risk of low energy availability.
If you fail to address low energy availability, it can develop into Relative Energy Deficiency in Sport (RED-S), a syndrome that affects many aspects of physiological function.
How to Calculate Energy Availability
You can calculate your energy availability using the following equation:
(Total Energy Intake – Exercise Expenditure) ÷ Fat-Free Mass in Kilograms
(Note: Fat-free mass refers to your total body weight minus the weight of your body that’s fat. You can calculate your fat-free mass using the calculator here.)
If you plug your numbers into this equation, you end up with your energy availability relative to your fat-free mass. We express this as a number of calories per kilogram of lean body mass per day, which we typically shorten to:
## kcals/kg of FFM/day
While the numbers are far from exact, most scientists agree that an energy availability of ~45 kcal/kg of FFM/day is optimal for health. In contrast, an energy availability of <30 kcal/kg of FFM/day constitutes low energy availability.
To better understand this, here’s an example using a weightlifter called Joe.
Joe weighs 80 kg (~176 lb.) and has 12% body fat. Thus, Joe has ~70 kg of fat-free mass.
He also eats 3,000 calories per day and burns 400 calories during his daily workouts, which means he has 2,600 calories remaining to fuel his bodily functions.
If we plug these numbers into the above equation, we get Joe’s energy availability relative to his fat-free mass:
(3,000 calories – 400 calories) ÷ 70 kg of Lean Mass = ~37 kcal/kg FFM/day
Based on these numbers, Joe is in a state of adequate energy availability, although probably not optimal for long-term health.
If he were to raise his calories to 3,500 per day and keep his activity levels the same, weight, and body composition the same, this would bump him up to 44 kcal/kg FFM/day.
If he were to slash his calories to 2,000 per day, this would drop his kcal/kg FFM/day to just 23. While this isn’t overly harmful for a few days or weeks, it could lead to symptoms associated with RED-S if maintained for long.
What Are the Symptoms of RED-S?
The most common RED-S symptoms include:
What Are the Health Implications of RED-S?
The diagram below shows how RED-S affects your health and performance.
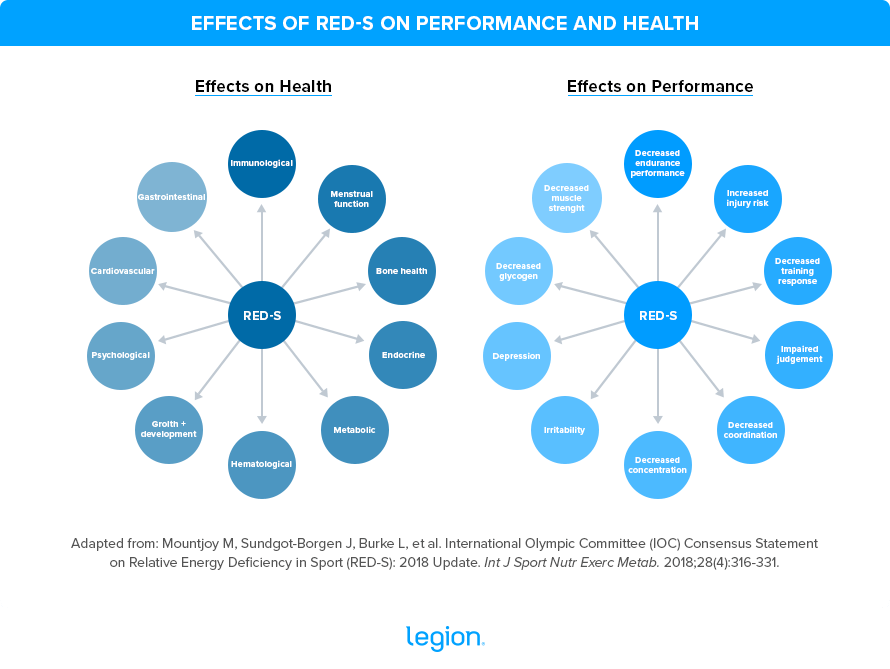
Let’s dig deeper into the most notable ways RED-S affects your physical and mental well-being.
Hormones
Low energy availability disrupts the hypothalamic–pituitary–gonadal axis, sometimes called the HPG axis, which regulates sex hormones such as estrogen and testosterone.
It also alters thyroid function, causes changes in appetite-regulating hormones (including decreasing leptin and oxytocin and increasing ghrelin, peptide YY, and adiponectin), reduces insulin and insulin-like growth factor 1 (IGF-1), increases growth hormone resistance, and elevates cortisol.
Your body likely actions these changes to conserve energy for more vital functions.
Menstrual Function
Low energy availability prevents the body from releasing the hormones that begin and advance the menstrual cycle, including gonadotropin-releasing hormone (GnRH), luteinizing hormone, and follicle-stimulating hormone.
This decreases estrogen and progesterone levels and causes hypothalamic amenorrhea, a condition in which the hypothalamus stops the menstrual cycle.
Bone Health
People with low energy availability typically have lower bone density than healthy people because they don’t produce enough of the hormones that orchestrate bone metabolism. These hormones regulate the production and degradation of bone and include IGF-1, leptin, triiodothyronine, testosterone, and estrogen.
Furthermore, people who intentionally restrict their calorie intake may not get sufficient calcium and vitamin D from their diet, both of which are vital for maintaining healthy bones.
This is significant because having low bone density can increase your risk of bone injuries such as stress fractures.
Metabolic Function
When you have low energy availability, your resting metabolic rate tends to drop. This is likely so your body can conserve energy for more vital functions.
Studies also show low energy availability is associated with increased body fat percentage and muscle breakdown. While fat gain in this scenario seems paradoxical, scientists have reported it in several studies, even those including people with anorexia.
Haematologic Function
Many athletes (especially females) are iron deficient, which can contribute to energy deficiency.
This is because iron-deficit people tend to have diminished appetite and eat less. They also have impaired metabolic function, causing them to burn more energy during exercise and at rest.
This has numerous effects throughout the body, including impairing bone health, thyroid function, fertility and psychological well-being.
Gastrointestinal Health
Gastrointestinal issues, such as constipation, bloating, abdominal pain, and fecal incontinence, can affect people with low energy availability.
Immune Function
Studies show that low energy availability hinders immune function and increases the likelihood of becoming ill.
For example, in a study conducted by scientists at the University of Tsukuba, researchers found that elite runners who were likely suffering from low energy availability were dogged by more upper respiratory tract infections (including symptoms such as sore throat, headache, runny nose, coughing, and fever) than those who weren’t energy deficient.
Cognition and Mental Health
Research shows that people with low energy availability have decreased cognitive ability and attention and an increased risk of anxiety and depression.
For example, in a study published in the British Journal of Sports Medicine, researchers found that people admitted to hospital with sports-related injuries and low energy availability were 4.3-times more likely to report impaired judgment, 1.6-times more likely to report feeling uncoordinated, and twice as likely to report problems concentrating than those admitted with adequate energy availability.
What Are the Performance Implications of RED-S?
There’s little long-term research investigating the effects of RED-S on athletic performance. Even without evidence, however, experts generally agree that there are several ways that RED-S could stop you from performing at your best.
For instance, low energy availability can hinder glycogen storage, making it difficult to train and compete at a high intensity. It also impairs muscle protein synthesis, which stymies your ability to build muscle.
Moreover, those with low energy availability are more likely to miss training through illness and injury, which could compromise performance over time.
Other research suggests that energy deficiency can hamper strength, endurance, reaction time, speed, and recovery. It’s also associated with higher cortisol levels, lower muscle mass, and diminished levels of blood glucose, triiodothyronine, and estrogen, all of which can fetter physical performance.
Given these factors, it’s little wonder why the athletes who likely have the lowest energy availability tend to be the ones who perform worst in competition.
How to Prevent and Treat RED-S
To prevent and treat RED-S, you must prioritize proper nutrition.
This means doing the following:
1. Eat sufficient calories: The basis of RED-S is energy deficiency. Thus, the best preventative measure and treatment is to eat enough calories every day, taking into account the number of calories you burn through exercise.
You can calculate how many calories you should eat based on your body composition goals and energy expenditure using the Legion Calorie Calculator here.
2. Eat sufficient protein: Protein is essential for muscle repair and growth. Most people who exercise regularly should eat 0.8-to-1.2 grams of protein per pound of body weight per day, depending on whether they want to gain or lose weight.
They may also choose to eat slightly more than this while recovering from injury since doing so can accelerate recovery and help you maintain muscle while you’re unable to train.
Supplementing with protein powder is a convenient way to help you hit your daily protein target. If you want a clean, 100% natural, delicious protein powder that’s naturally sweetened and flavored and contains no artificial dyes or other chemical junk, try Whey+ or Casein+.
(Or if you aren’t sure if Whey+ protein powder or Casein+ protein powder is right for you, take the Legion Supplement Finder Quiz! In less than a minute, it’ll tell you exactly what supplements are right for you. Click here to check it out.)
3. Eat sufficient carbohydrates: Carbohydrates provide fuel for your body during exercise. Research suggests that physically active people should eat ~2.2-to-5.5 grams of carbs per pound of body weight per day, depending on how hard and long they train.
Those training at moderate-to-high intensities for 1-to-3 hours per day should consume closer to ~2.2-to-4 grams per pound of body weight per day, whereas those training at moderate-to-high intensities 4-to-5 hours per day should consume closer to ~4-to-5.5 grams per pound of body weight per day.
4. Eat sufficient fat: Dietary fat is a critical component of your body’s cells and contributes to several aspects of your general health, including immune function, nutrient absorption, and hormone regulation.
Aim to get 15-to-30% of your daily calories from fat.
5. Prioritize nutritious foods: Eating vitamin- and nutrient-dense foods helps you avoid becoming deficient in micronutrients such as calcium, phosphorus, iron, and vitamin D that can exacerbate RED-S.
Supplementing with a multivitamin can also help.
If you want a multivitamin containing clinically effective doses of 31 vitamins and minerals designed to plug the most common holes in an athlete’s diet, enhance your health and mood, and reduce stress, fatigue, and anxiety, try Triumph for men and women.
6. Follow a well-designed training program: Your training program should contain the right amount of weekly exercise to spur progress, but not so much that you run yourself ragged.
If you want a training program that does just that, check out my best-selling fitness books Bigger Leaner Stronger for men and Thinner Leaner Stronger for women.
(If you aren’t sure if Bigger Leaner Stronger or Thinner Leaner Stronger is right for you or if another strength training program might be a better fit for your circumstances and goals, take Legion Strength Training Quiz, and in less than a minute, you’ll know the perfect strength training program for you. Click here to check it out.)
+ Scientific References
- Wasserfurth, P., Palmowski, J., Hahn, A., & Krüger, K. (2020). Reasons for and Consequences of Low Energy Availability in Female and Male Athletes: Social Environment, Adaptations, and Prevention. Sports Medicine – Open, 6(1). https://doi.org/10.1186/S40798-020-00275-6
- Mountjoy, M., Sundgot-Borgen, J. K., Burke, L. M., Ackerman, K. E., Blauwet, C., Constantini, N., Lebrun, C., Lundy, B., Melin, A. K., Meyer, N. L., Sherman, R. T., Tenforde, A. S., Torstveit, M. K., & Budgett, R. (2018). IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. British Journal of Sports Medicine, 52(11), 687–697. https://doi.org/10.1136/BJSPORTS-2018-099193
- Azizi, M. K., Shariff, N. M., Yusof, A., & Azizan, N. A. (2021). A Narrative Review of Low Energy Availability. Malaysian Journal of Medicine and Health Sciences, 17(SUPP9), 189–194.
- Wasserfurth, P., Palmowski, J., Hahn, A., & Krüger, K. (2020). Reasons for and Consequences of Low Energy Availability in Female and Male Athletes: Social Environment, Adaptations, and Prevention. Sports Medicine – Open 2020 6:1, 6(1), 1–14. https://doi.org/10.1186/S40798-020-00275-6
- Loucks, A. B., & Thuma, J. R. (2003). Luteinizing hormone pulsatility is disrupted at a threshold of energy availability in regularly menstruating women. The Journal of Clinical Endocrinology and Metabolism, 88(1), 297–311. https://doi.org/10.1210/JC.2002-020369
- Allaway, H. C. M., Southmayd, E. A., & De Souza, M. J. (2016). The physiology of functional hypothalamic amenorrhea associated with energy deficiency in exercising women and in women with anorexia nervosa. Hormone Molecular Biology and Clinical Investigation, 25(2), 91–119. https://doi.org/10.1515/HMBCI-2015-0053
- Ihle, R., & Loucks, A. B. (2004). Dose-response relationships between energy availability and bone turnover in young exercising women. Journal of Bone and Mineral Research : The Official Journal of the American Society for Bone and Mineral Research, 19(8), 1231–1240. https://doi.org/10.1359/JBMR.040410
- Logue, D., Madigan, S. M., Delahunt, E., Heinen, M., Mc Donnell, S. J., & Corish, C. A. (2018). Low Energy Availability in Athletes: A Review of Prevalence, Dietary Patterns, Physiological Health, and Sports Performance. Sports Medicine (Auckland, N.Z.), 48(1), 73–96. https://doi.org/10.1007/S40279-017-0790-3
- Misra, M. (2014). Neuroendocrine mechanisms in athletes. Handbook of Clinical Neurology, 124, 373–386. https://doi.org/10.1016/B978-0-444-59602-4.00025-3
- Jasienska, G. (2003). Energy metabolism and the evolution of reproductive suppression in the human female. Acta Biotheoretica, 51(1), 1–18. https://doi.org/10.1023/A:1023035321162
- Wade, G. N., & Jones, J. E. (2004). Neuroendocrinology of nutritional infertility. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, 287(6). https://doi.org/10.1152/AJPREGU.00475.2004
- Gordon, C. M., Ackerman, K. E., Berga, S. L., Kaplan, J. R., Mastorakos, G., Misra, M., Murad, M. H., Santoro, N. F., & Warren, M. P. (2017). Functional Hypothalamic Amenorrhea: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology and Metabolism, 102(5), 1413–1439. https://doi.org/10.1210/JC.2017-00131
- Curry, E. J., Logan, C., Ackerman, K., McInnis, K. C., & Matzkin, E. G. (2015). Female Athlete Triad Awareness Among Multispecialty Physicians. Sports Medicine – Open, 1(1). https://doi.org/10.1186/S40798-015-0037-5
- Southmayd, E. A., Williams, N. I., Mallinson, R. J., & De Souza, M. J. (2019). Energy Deficiency Suppresses Bone Turnover in Exercising Women With Menstrual Disturbances. The Journal of Clinical Endocrinology and Metabolism, 104(8), 3131–3145. https://doi.org/10.1210/JC.2019-00089
- Papageorgiou, M., Dolan, E., Elliott-Sale, K. J., & Sale, C. (2018). Reduced energy availability: implications for bone health in physically active populations. European Journal of Nutrition, 57(3), 847–859. https://doi.org/10.1007/S00394-017-1498-8
- De Souza, M. J., West, S. L., Jamal, S. A., Hawker, G. A., Gundberg, C. M., & Williams, N. I. (2008). The presence of both an energy deficiency and estrogen deficiency exacerbate alterations of bone metabolism in exercising women. Bone, 43(1), 140–148. https://doi.org/10.1016/J.BONE.2008.03.013
- Duckham, R. L., Peirce, N., Bailey, C. A., Summers, G., Cameron, N., & Brooke-Wavell, K. (2013). Bone geometry according to menstrual function in female endurance athletes. Calcified Tissue International, 92(5), 444–450. https://doi.org/10.1007/S00223-013-9700-3
- Southmayd, E. A., Mallinson, R. J., Williams, N. I., Mallinson, D. J., & De Souza, M. J. (2017). Unique effects of energy versus estrogen deficiency on multiple components of bone strength in exercising women. Osteoporosis International : A Journal Established as Result of Cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 28(4), 1365–1376. https://doi.org/10.1007/S00198-016-3887-X
- Sundgot-Borgen, J., & Torstveit, M. K. (2007). The female football player, disordered eating, menstrual function and bone health. British Journal of Sports Medicine, 41 Suppl 1(Suppl 1). https://doi.org/10.1136/BJSM.2007.038018
- Beals, K. A., & Mitchell, A. (2013). Recent Recommendations and Current Controversies in Sport Nutrition. Http://Dx.Doi.Org/10.1177/1559827613513410, 9(4), 288–297. https://doi.org/10.1177/1559827613513410
- Tenforde, A. S., Carlson, J. L., Chang, A., Sainani, K. L., Shultz, R., Kim, J. H., Cutti, P., Golden, N. H., & Fredericson, M. (2017). Association of the Female Athlete Triad Risk Assessment Stratification to the Development of Bone Stress Injuries in Collegiate Athletes. The American Journal of Sports Medicine, 45(2), 302–310. https://doi.org/10.1177/0363546516676262
- Fujita, S., Sakuraba, K., Kubota, A., Wakamatsu, K., & Koikawa, N. (2017). Stress Fracture Influences Bone Resorption marker (u-NTX) in Female Long Distance Runners. International Journal of Sports Medicine, 38(14), 1070–1075. https://doi.org/10.1055/S-0043-119223
- Elliott-Sale, K. J., Tenforde, A. S., Parziale, A. L., Holtzman, B., & Ackerman, K. E. (2018). Endocrine Effects of Relative Energy Deficiency in Sport. International Journal of Sport Nutrition and Exercise Metabolism, 28(4), 335–349. https://doi.org/10.1123/IJSNEM.2018-0127
- Wade, G. N., & Schneider, J. E. (1992). Metabolic fuels and reproduction in female mammals. Neuroscience and Biobehavioral Reviews, 16(2), 235–272. https://doi.org/10.1016/S0149-7634(05)80183-6
- Wade, G. N., Schneider, J. E., & Li, H. Y. (1996). Control of fertility by metabolic cues. Https://Doi.Org/10.1152/Ajpendo.1996.270.1.E1, 270(1 33-1). https://doi.org/10.1152/AJPENDO.1996.270.1.E1
- Deutz, R. C., Benardot, D., Martin, D. E., & Cody, M. M. (2000). Relationship between energy deficits and body composition in elite female gymnasts and runners. Medicine and Science in Sports and Exercise, 32(3), 659–668. https://doi.org/10.1097/00005768-200003000-00017
- Zamboni, M., Armellini, F., Turcato, E., Todisco, P., Gallagher, D., Dalle Grave, R., Heymsfield, S., & Bosello, O. (1997). Body fat distribution before and after weight gain in anorexia nervosa. International Journal of Obesity 1997 21:1, 21(1), 33–36. https://doi.org/10.1038/sj.ijo.0800357
- Lackner, S., Mörkl, S., Müller, W., Fürhapter-Rieger, A., Oberascher, A., Lehofer, M., Bieberger, C., Wonisch, W., Amouzadeh-Ghadikolai, O., Moser, M., Mangge, H., Zelzer, S., & Holasek, S. J. (2019). Novel approaches for the assessment of relative body weight and body fat in diagnosis and treatment of anorexia nervosa: A cross-sectional study. Clinical Nutrition (Edinburgh, Scotland), 38(6), 2913–2921. https://doi.org/10.1016/J.CLNU.2018.12.031
- Hübel, C., Yilmaz, Z., Schaumberg, K. E., Breithaupt, L., Hunjan, A., Horne, E., García-González, J., O’Reilly, P. F., Bulik, C. M., & Breen, G. (2019). Body composition in anorexia nervosa: Meta-analysis and meta-regression of cross-sectional and longitudinal studies. The International Journal of Eating Disorders, 52(11), 1205–1223. https://doi.org/10.1002/EAT.23158
- Fazeli, P. K., & Klibanski, A. (2019). The paradox of marrow adipose tissue in anorexia nervosa. Bone, 118, 47–52. https://doi.org/10.1016/J.BONE.2018.02.013
- Fazeli, P. K., Faje, A. T., Bredella, M. A., Polineni, S., Russell, S., Resulaj, M., Rosen, C. J., & Klibanski, A. (2019). Changes in marrow adipose tissue with short-term changes in weight in premenopausal women with anorexia nervosa. European Journal of Endocrinology, 180(3), 189–199. https://doi.org/10.1530/EJE-18-0824
- Clénin, G. E., Cordes, M., Huber, A., Schumacher, Y., Noack, P., Scales, J., & Kriemler, S. (2015). Iron deficiency in sports – definition, influence on performance and therapy. Swiss Medical Weekly, 145(1), 6–18. https://doi.org/10.4414/SMW.2015.14196
- Petkus, D. L., Murray-Kolb, L. E., & De Souza, M. J. (2017). The Unexplored Crossroads of the Female Athlete Triad and Iron Deficiency: A Narrative Review. Sports Medicine (Auckland, N.Z.), 47(9), 1721–1737. https://doi.org/10.1007/S40279-017-0706-2
- Norris, M. L., Harrison, M. E., Isserlin, L., Robinson, A., Feder, S., & Sampson, M. (2016). Gastrointestinal complications associated with anorexia nervosa: A systematic review. The International Journal of Eating Disorders, 49(3), 216–237. https://doi.org/10.1002/EAT.22462
- Melin, A., Tornberg, Å. B., Skouby, S., Faber, J., Ritz, C., Sjödin, A., & Sundgot-Borgen, J. (2014). The LEAF questionnaire: a screening tool for the identification of female athletes at risk for the female athlete triad. British Journal of Sports Medicine, 48(7), 540–545. https://doi.org/10.1136/BJSPORTS-2013-093240
- Ackerman, K. E., Holtzman, B., Cooper, K. M., Flynn, E. F., Bruinvels, G., Tenforde, A. S., Popp, K. L., Simpkin, A. J., & Parziale, A. L. (2019). Low energy availability surrogates correlate with health and performance consequences of Relative Energy Deficiency in Sport. British Journal of Sports Medicine, 53(10), 628–633. https://doi.org/10.1136/BJSPORTS-2017-098958
- Drew, M., Vlahovich, N., Hughes, D., Appaneal, R., Burke, L. M., Lundy, B., Rogers, M., Toomey, M., Watts, D., Lovell, G., Praet, S., Halson, S. L., Colbey, C., Manzanero, S., Welvaert, M., West, N. P., Pyne, D. B., & Waddington, G. (2018). Prevalence of illness, poor mental health and sleep quality and low energy availability prior to the 2016 Summer Olympic Games. British Journal of Sports Medicine, 52(1), 47–53. https://doi.org/10.1136/BJSPORTS-2017-098208
- Drew, M. K., Vlahovich, N., Hughes, D., Appaneal, R., Peterson, K., Burke, L., Lundy, B., Toomey, M., Watts, D., Lovell, G., Praet, S., Halson, S., Colbey, C., Manzanero, S., Welvaert, M., West, N., Pyne, D. B., & Waddington, G. (2017). A multifactorial evaluation of illness risk factors in athletes preparing for the Summer Olympic Games. Journal of Science and Medicine in Sport, 20(8), 745–750. https://doi.org/10.1016/J.JSAMS.2017.02.010
- Shimizu, K., Suzuki, N., Nakamura, M., Aizawa, K., Imai, T., Suzuki, S., Eda, N., Hanaoka, Y., Nakao, K., Suzuki, N., Mesaki, N., Kono, I., & Akama, T. (2012). Mucosal immune function comparison between amenorrheic and eumenorrheic distance runners. Journal of Strength and Conditioning Research, 26(5), 1402–1406. https://doi.org/10.1519/JSC.0B013E31822E7A6C
- Sundgot-Borgen, J., & Torstveit, M. K. (2010). Aspects of disordered eating continuum in elite high-intensity sports. Scandinavian Journal of Medicine & Science in Sports, 20 Suppl 2(SUPPL. 2), 112–121. https://doi.org/10.1111/J.1600-0838.2010.01190.X
- Petkus, D. L., Murray-Kolb, L. E., & De Souza, M. J. (2017). The Unexplored Crossroads of the Female Athlete Triad and Iron Deficiency: A Narrative Review. Sports Medicine (Auckland, N.Z.), 47(9), 1721–1737. https://doi.org/10.1007/S40279-017-0706-2
- Thein-Nissenbaum, J. M., & Carr, K. E. (2011). Female athlete triad syndrome in the high school athlete. Physical Therapy in Sport : Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, 12(3), 108–116. https://doi.org/10.1016/J.PTSP.2011.04.002
- Javed, A., Tebben, P. J., Fischer, P. R., & Lteif, A. N. (2013). Female athlete triad and its components: toward improved screening and management. Mayo Clinic Proceedings, 88(9), 996–1009. https://doi.org/10.1016/J.MAYOCP.2013.07.001
- Ackerman, K. E., Holtzman, B., Cooper, K. M., Flynn, E. F., Bruinvels, G., Tenforde, A. S., Popp, K. L., Simpkin, A. J., & Parziale, A. L. (2019). Low energy availability surrogates correlate with health and performance consequences of Relative Energy Deficiency in Sport. British Journal of Sports Medicine, 53(10), 628–633. https://doi.org/10.1136/BJSPORTS-2017-098958
- Tarnopolsky, M. A., Zawada, C., Richmond, L. B., Carter, S., Shearer, J., Graham, T., & Phillips, S. M. (2001). Gender differences in carbohydrate loading are related to energy intake. Journal of Applied Physiology (Bethesda, Md. : 1985), 91(1), 225–230. https://doi.org/10.1152/JAPPL.2001.91.1.225
- Areta, J. L., Burke, L. M., Camera, D. M., West, D. W. D., Crawshay, S., Moore, D. R., Stellingwerff, T., Phillips, S. M., Hawley, J. A., & Coffey, V. G. (2014). Reduced resting skeletal muscle protein synthesis is rescued by resistance exercise and protein ingestion following short-term energy deficit. American Journal of Physiology. Endocrinology and Metabolism, 306(8). https://doi.org/10.1152/AJPENDO.00590.2013
- Raysmith, B. P., & Drew, M. K. (2016). Performance success or failure is influenced by weeks lost to injury and illness in elite Australian track and field athletes: A 5-year prospective study. Journal of Science and Medicine in Sport, 19(10), 778–783. https://doi.org/10.1016/J.JSAMS.2015.12.515
- Woods, A. L., Garvican-Lewis, L. A., Lundy, B., Rice, A. J., & Thompson, K. G. (2017). New approaches to determine fatigue in elite athletes during intensified training: Resting metabolic rate and pacing profile. PloS One, 12(3). https://doi.org/10.1371/JOURNAL.PONE.0173807
- Tornberg, Å. B., Melin, A., Koivula, F. M., Johansson, A., Skouby, S., Faber, J., & Sjödin, A. (2017). Reduced Neuromuscular Performance in Amenorrheic Elite Endurance Athletes. Medicine and Science in Sports and Exercise, 49(12), 2478–2485. https://doi.org/10.1249/MSS.0000000000001383
- Mooses, M., & Hackney, A. C. (2017). Anthropometrics and Body Composition in East African Runners: Potential Impact on Performance. International Journal of Sports Physiology and Performance, 12(4), 422–430. https://doi.org/10.1123/IJSPP.2016-0408
- Vanheest, J. L., Rodgers, C. D., Mahoney, C. E., & De Souza, M. J. (2014). Ovarian suppression impairs sport performance in junior elite female swimmers. Medicine and Science in Sports and Exercise, 46(1), 156–166. https://doi.org/10.1249/MSS.0B013E3182A32B72
- Silva, M. R. G., & Paiva, T. (2016). Poor precompetitive sleep habits, nutrients’ deficiencies, inappropriate body composition and athletic performance in elite gymnasts. European Journal of Sport Science, 16(6), 726–735. https://doi.org/10.1080/17461391.2015.1103316
- Tipton, K. D. (2015). Nutritional Support for Exercise-Induced Injuries. Sports Medicine (Auckland, N.Z.), 45 Suppl 1, 93–104. https://doi.org/10.1007/S40279-015-0398-4
- Wall, B. T., Morton, J. P., & van Loon, L. J. C. (2015). Strategies to maintain skeletal muscle mass in the injured athlete: nutritional considerations and exercise mimetics. European Journal of Sport Science, 15(1), 53–62. https://doi.org/10.1080/17461391.2014.936326
- Bytomski, J. R. (2018). Fueling for Performance. Sports Health, 10(1), 47–53. https://doi.org/10.1177/1941738117743913
- Shaw, G., Serpell, B., & Baar, K. (2019). Rehabilitation and nutrition protocols for optimising return to play from traditional ACL reconstruction in elite rugby union players: A case study. Journal of Sports Sciences, 37(15), 1794–1803. https://doi.org/10.1080/02640414.2019.1594571
- Stellingwerff, T., Maughan, R. J., & Burke, L. M. (2011). Nutrition for power sports: middle-distance running, track cycling, rowing, canoeing/kayaking, and swimming. Journal of Sports Sciences, 29 Suppl 1(SUPPL. 1). https://doi.org/10.1080/02640414.2011.589469
- Stellingwerff, T., Bovim, I. M., & Whitfield, J. (2019). Contemporary Nutrition Interventions to Optimize Performance in Middle-Distance Runners. International Journal of Sport Nutrition and Exercise Metabolism, 29(2), 106–116. https://doi.org/10.1123/IJSNEM.2018-0241
- Burke, L. M., Jones, A. M., Jeukendrup, A. E., & Mooses, M. (2019). Contemporary Nutrition Strategies to Optimize Performance in Distance Runners and Race Walkers. International Journal of Sport Nutrition and Exercise Metabolism, 29(2), 117–129. https://doi.org/10.1123/IJSNEM.2019-0004
[ad_2]
Source link



