[ad_1]
Historically, physician administered specialty pharmaceuticals are covered by a patient’s medical benefit and oral medications are covered by the pharmacy benefit. Increasingly, however, specialty pharmaceuticals are being covered by pharmaceutical benefits. Does this make a difference? Does medical vs. pharmacy coverage of drugs impact patient access?
A recent paper by Levine et al. (2023) aims to answer this question. They use data from the Tufts Medical Center Specialty Drug Evidence and Coverage Database. This database includes coverage policies from 17 large US commercial health plans. They find the following:
RESULTS: Eight plans issued separate medical and pharmacy benefit coverage policies for the same specialty drug and indication. Among these 8 plans, we identified 1,619 medical-pharmacy policy pairs. Eighty-six percent of pairs were concordant (1,386/1,619), and 14% were discordant (233/1,619). Discordance was most often due to differences in plans’ application of step therapy protocols (184/233), followed by prescriber requirements (52/233) and patient subgroups (25/233). Forty pairs were discordant in multiple ways. Of discordant pairs, medical policies were more restrictive 41% (96/233) of the time; pharmacy policies were more restrictive 54% (125/233) of the time; 5% of the time (12/233), the medical policy was more restrictive in some ways, but the pharmacy policy was more restrictive in others. Overall, plans imposed coverage restrictions in their medical and pharmacy policies with similar frequencies.
CONCLUSIONS: Commercial health plans’ medical and pharmacy coverage policies for the same specialty drugs tended to be concordant, although we found coverage criteria to be discordant 14% of the time. Medical and pharmacy policies that are inconsistent in their coverage criteria and restrictions complicate, and potentially hinder, patients’ access to specialty drugs.
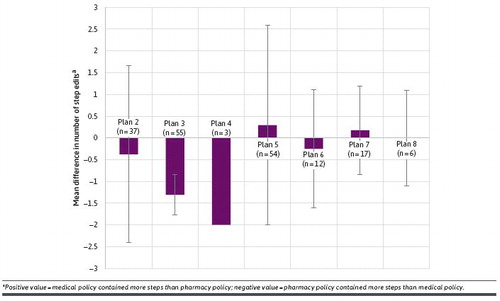
As shown in the table below, the number of step edits varied across the medial vs. pharmacy benefits.
The full article is here.
[ad_2]
Source link



