That is the answer Caswell-Jin et al. (2024) aim to answer. The authors used 4 cancer mortality models within CISNET for this study:
- Model D (Dana-Farber Cancer Institute). Used to define a set of disease states and implemented analytic formulations to estimate the association of interventions on transitions between these states, as well as on breast cancer incidence and mortality.
- Model M (MD Anderson Cancer Center). Relied on a a bayesian approach, which asseded the probability distributions for unknown parameters, including treatment benefits, and fitting to observed breast cancer mortality
- model S (Stanford University). A microsimulation that modelled natural history of disease based on tumor size and stage progression mapped to detection; treatments benefits were applied to baseline survival curves based on stage, age, and estrogen receptor (ER)/ERBB2 (formerly HER2) status at detection.
- model W (University of Wisconsin–Harvard). This model used a tumor growth framework and was calibrated incidence and mortality based on Surveillance, Epidemiology, and End Results Program (SEER) registry. This model also incorporated a cure fraction.
Categories of breast cancer by ER/ERBB2 status (ER+/ERBB2−, ER+/ERBB2+, ER−/ERBB2+, and ER−/ERBB2−) were modelled separately.
Using this approach, the authors found that:
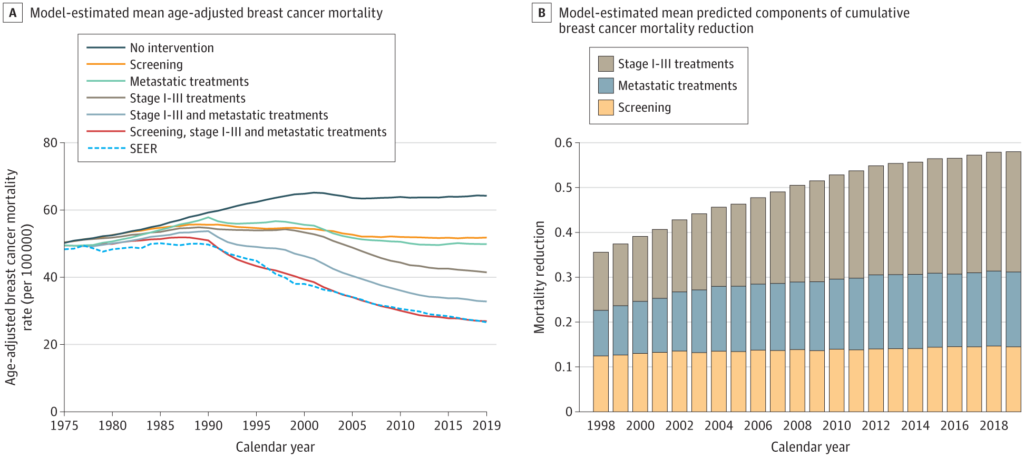
The breast cancer mortality rate in the US (age adjusted) was 48/100 000 women in 1975 and 27/100 000 women in 2019. In 2019, the combination of screening, stage I to III treatment, and metastatic treatment was associated with a 58% reduction (model range, 55%-61%) in breast cancer mortality. Of this reduction, 29% (model range, 19%-33%) was associated with treatment of metastatic breast cancer, 47% (model range, 35%-60%) with treatment of stage I to III breast cancer, and 25% (model range, 21%-33%) with mammography screening. Based on simulations, the greatest change in survival after metastatic recurrence occurred between 2000 and 2019, from 1.9 years (model range, 1.0-2.7 years) to 3.2 years (model range, 2.0-4.9 years).
You can read the full paper here.

