[ad_1]
The Oncology Care Model (OCM) is dead. The Oncology Care Model was a voluntary, alternative payment model (APM), that “included financial and performance accountability for episodes of care surrounding chemotherapy administration to cancer patients.” OCM expired at the end of June 2022, and will be replaced by the Enhancing Oncology Model. EOM is also a voluntary model that will run for 5 years: July 2023 through June 2028. [Note: Yes, there is a 1 year gap between the end of OCM and the start of EOM]
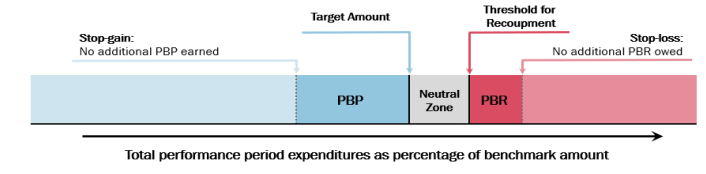
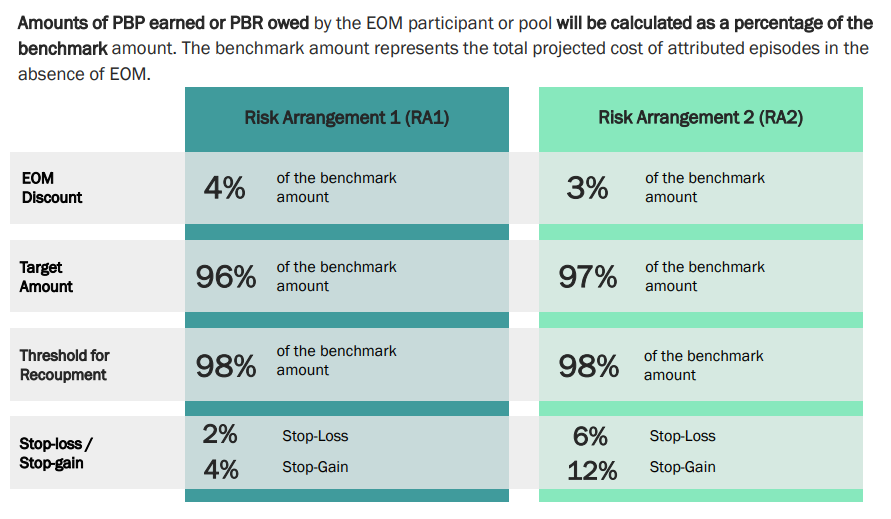
Like OCM, EOM allows both oncology physician group practices (PGPs) as well as other payers (eg, commercial payers, state Medicaid agencies) to participate in EOM–the latter through multi-payer agreements. Like OCM, under EOM physicians are paid an additional monthly fee to provide coordinated care to their cancer patients. Like OCM, EOM will measure value for cancer patients based on six-month episodes of care where the initiation of chemotherapy (or similar targeted therapies) will be the initiating point of the episode. Like OCM, EOM physicians are eligible for retrospective performance-based payment (PBP) based on quality of care and cost savings during these six month episodes of care (see EOM Fact Sheet, CMS slides). The way cost savings bonuses and penalties are calculated are shown in the figures below.
There are seven types of cancer that are included in EOM. These include the following tumor types:
- breast cancer,
- chronic leukemia,
- Small intestine/colorectal cancer,
- lung cancer,
- lymphoma,
- multiple myeloma,
- Prostate cancer
Patients are attributed to PGP based on the share of evaluation and management (E&M) services provided between initiating chemotherapy and the 6-month episodes. The PGP must provide at least 25% of all cancer-related E&M services during the episode to be attributed the episode.
Unlike the OCM program, however, the EOM monthly payments are less generous. Medscape reports that “the CMS Innovation Center plans to cut the Monthly Enhanced Oncology Services payments in the EOM by more than half ($70 vs $160 for the OCM), but at the same time, expects more work from practices.” Note that the dually eligible individuals receive an additional MEOS payment of $30 (ie, $100 total) per month. The additional work includes additional data collection such as “collection of electronic patient-reported outcomes (ePROs), and screening for social needs that may affect treatment, such as transportation issues and nutritional needs.” While collecting these data is certainly a good thing, it’s not clear if EOM will provide sufficient funding for health systems to collect these data. Further, physician group practices must offer “24/7 access to a clinician, patient navigation services.”
On the positive side, HHS has stated that it will “encourage other payers (eg, commercial payers, state Medicaid agencies) to align with its core concepts to promote a consistent approach across payers and EOM participants’ patient population.” This could reduce the burden on physicians, hospitals and health systems to have to deal with different programs across different payer types.
Quality of care will be measured based on the following domains:
- Patient experience
- Avoidable acute care utilization
- Management of toxic symptoms
- Management of psychosocial health
- Management of end-of-life care
[ad_2]
Source link

