A Health Affairs Forefront article by Johnson and Dieleman (2022) published last week using the Centers for Medicare and Medicaid Services’ (CMS’s) State Health Expenditure Accounts (SHEA) data. A previous study looked at these data through 2014, but the recent publication updates this analysis through 2019. The authors first use an age- and sex-standardized health spending per person and adjust for inflation and regional price parity using data from the Bureau of Economic Analysis (BEA). Then, they apply a regression based approach to control for state differences in per capita income, population density, behavioral health risk, and time (which the authors define as the tendency of health spending to increase each year across all states).
Using this method, they find that:
…almost half of the variation in state health care spending was explained by income and regional prices. These two factors alongside time, health risks (physical activity and smoking prevalence), population density, age, and sex explained more than 75 percent of the variation
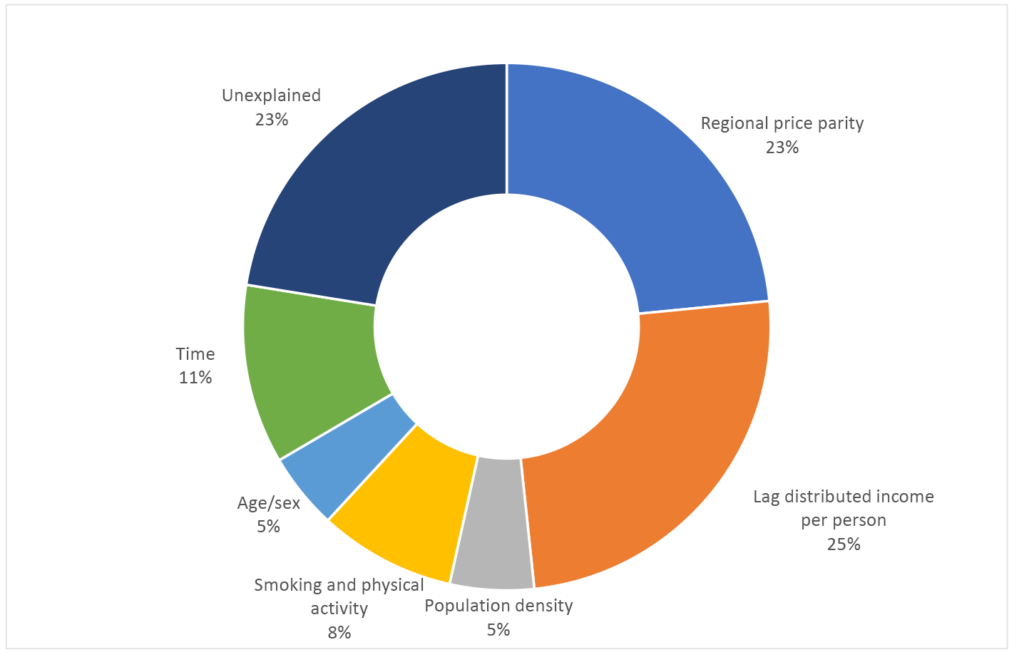
In other words, 23% of the variation in health care spending across states remains unexplained.
The authors also examined how Medicaid eligibility expansion enacted under the Affordable Care Act affected spending. The authors find that:
…increasing [Medicaid] income eligibility thresholds for children and adults was significantly associated with higher total health spending, but that increasing eligibility thresholds for pregnant women was associated with lower total spending… Medicaid expansion in any state led to 2 percent higher total spending in subsequent years compared to non- expansion states.
Read the full article here.

