[ad_1]
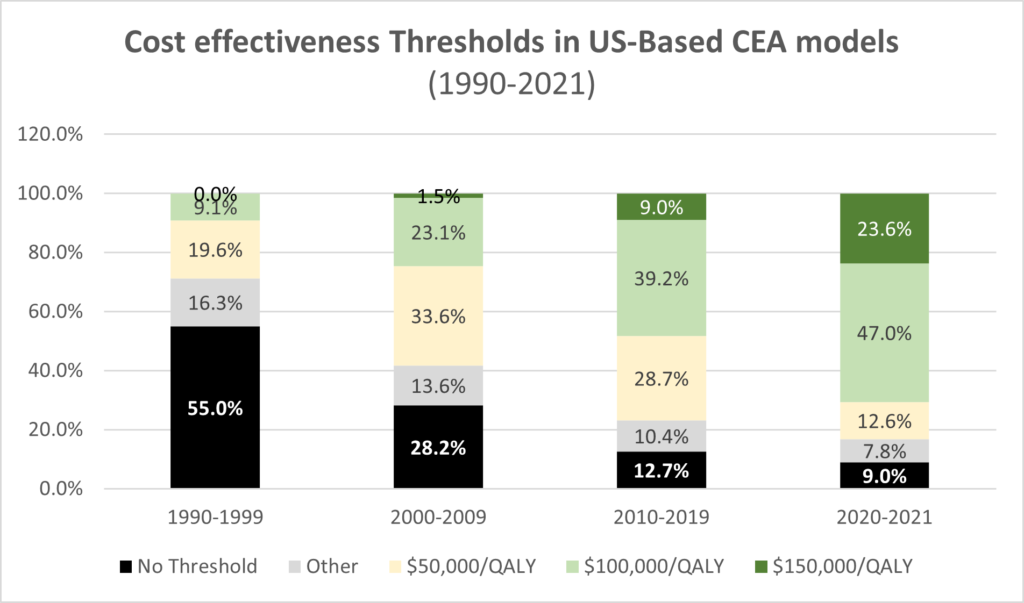
That is the question Peter Neumann and David Kim (2023) answer in their JAMA research letter published today. They use 1990-2021 data from the Tufts Medical Center CEA Registry. The results are summarized in the graphs below.
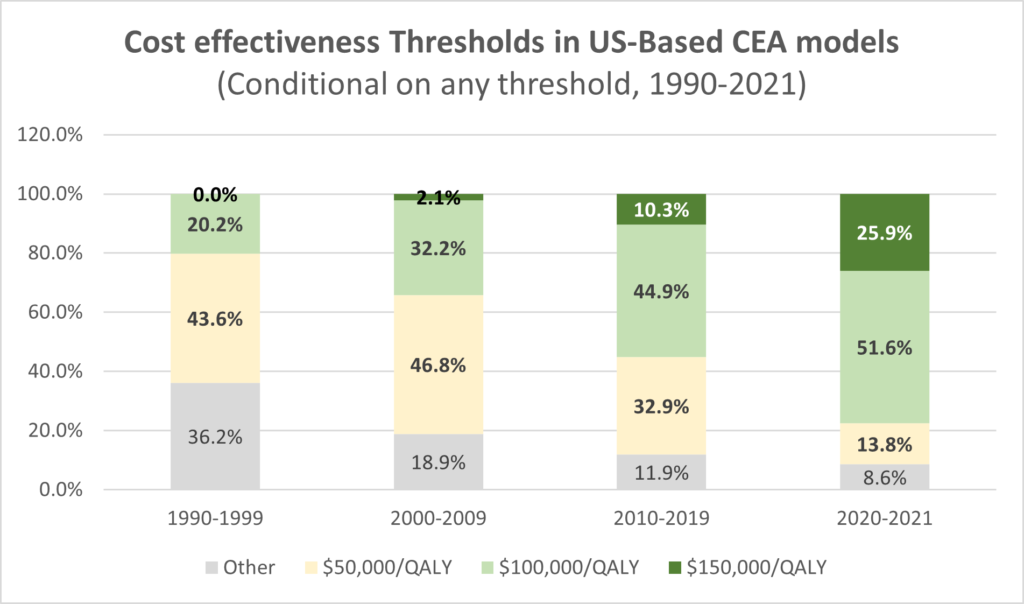
First, we see the use of an explicit cost effectiveness threshold increasing over time, from only 45% of published studies to 91% of all studies. Second, the cost-effectiveness thresholds have increased over time. Whereas 43.6% of studies reporting a CEA threshold used a $50,000/QALY threshold in the 1990s, now only 13.8% of studies use that threshold; whereas 0% of studies used the $150,000/QALY threshold in the 1990s, now 25.9% of studies do so.
The authors also note that:
- Cancer-related CEAs referenced higher thresholds than non-cancer CEAs, which may suggest a view that interventions for diseases associated with greater mortality and morbidity warrant higher thresholds.
- Authors of industry-funded analyzes tend to reference higher thresholds.
You can read the full paper here.
[ad_2]
Source link



